Sleep Apnea Simplified: What is it, Causes, Risks, and Modern Treatments

Sleep is crucial for health, yet countless individuals experience sleep apnea, a condition that can be disruptive and pose serious health risks. Despite its widespread occurrence, awareness of its causes, risks, and current treatment options remains limited. This article explains sleep apnea clearly, detailing its impact on the body and potential solutions.
What is Sleep Apnea?
Sleep apnea is a sleep disorder characterized by repeated interruptions in breathing during sleep. The most common form, obstructive sleep apnea (OSA), occurs when the upper airway repeatedly collapses or narrows during sleep, reducing or completely blocking airflow. These pauses may last 10 seconds or longer and can happen several times an hour, leading to fragmented sleep and decreased oxygen levels1.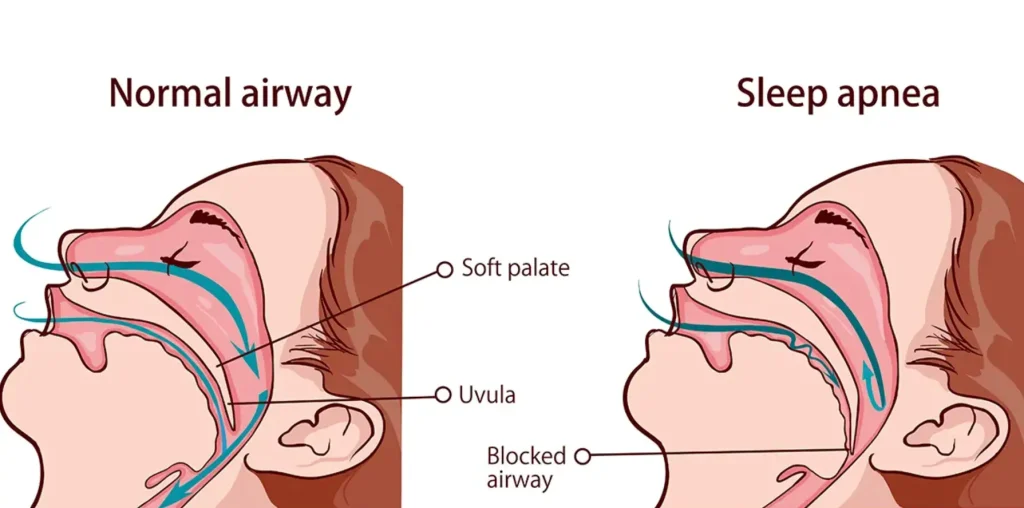
Causes of Sleep Apnea: The Science Behind the Blockage
Sleep apnea is a multifactorial condition influenced by various physiological factors. The primary cause is upper airway collapsibility. During sleep, muscles that generally keep the airway open relax. In individuals with OSA, this relaxation leads to airway collapse, particularly in the throat region. A key contributor is pharyngeal dilator muscle dysfunction—the failure of muscles that maintain airway openness during sleep. Anatomical features such as large tonsils, excess neck fat, or a small jaw can further narrow the airway2. Another critical factor is the arousal threshold, referring to how easily a person wakes in response to breathing difficulty. Some individuals awaken easily during minor airway obstruction, while others have a higher threshold, potentially worsening oxygen deprivation3. The ventilatory control system also plays a role. A highly sensitive or unstable ventilatory system (high loop gain) can amplify breathing disturbances, creating a cycle of apnea and fragmented sleep.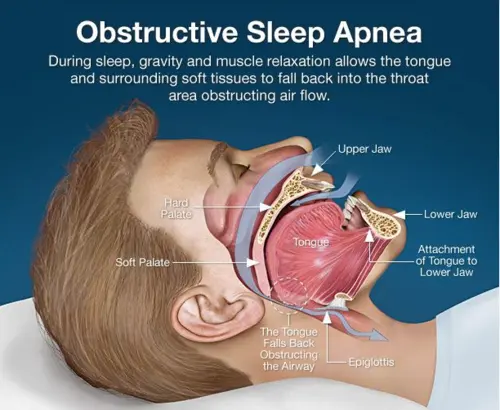
Risks and Consequences of Untreated Sleep Apnea
If left untreated, sleep apnea can lead to serious health complications:- Cardiovascular problems: Intermittent drops in oxygen levels and frequent awakenings increase the risk of hypertension, heart attacks, strokes, and arrhythmias4.
- Metabolic issues: Sleep apnea is linked to insulin resistance and type 2 diabetes5.
- Cognitive decline: Poor sleep quality contributes to memory problems, mood disorders, and decreased concentration.
- Daytime sleepiness: Increased fatigue heightens the likelihood of accidents, particularly during driving.
- Overall reduced quality of life: Ongoing fatigue impacts work, relationships, and mental well-being.

Diagnosing Sleep Apnea
It involves a sleep study known as polysomnography. This study monitors physiological parameters during sleep, including breathing, oxygen levels, and brain activity. Key diagnostic metrics consist of the apnea-hypopnea index (AHI), which measures the frequency of apnea and hypopnea events per hour of sleep6.Modern Treatments for Sleep Apnea
1)Continuous Positive Airway Pressure (CPAP)
CPAP remains one of the most effective treatments for moderate to severe obstructive sleep apnoea (OSA). It provides a continuous flow of pressurized air via a mask, functioning as a support to maintain the upper airway’s openness and prevent collapse. CPAP significantly decreases apnoea occurrences, enhances oxygen levels, and reduces daytime drowsiness. Although effective, patient compliance faces discomfort, claustrophobia, and inconvenience. Research indicates that 43% to 86% of patients have difficulty using CPAP consistently7.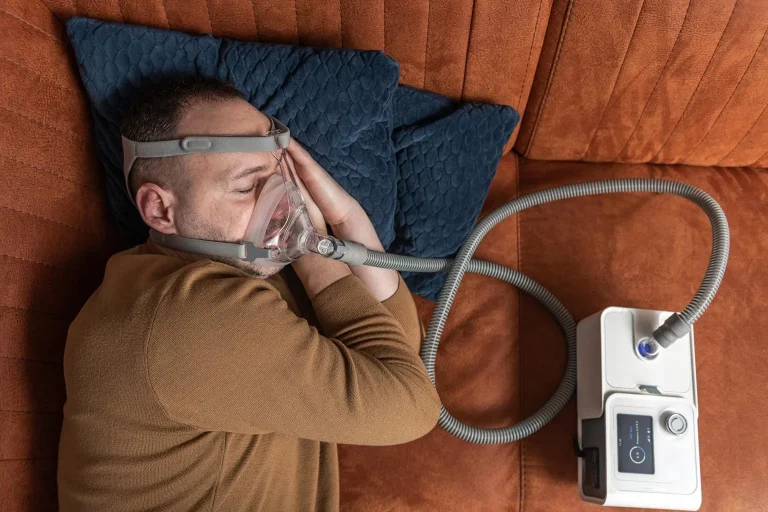
2)iNAP Therapy
iNAP (intermittent negative airway pressure) is a novel alternative to CPAP that gently applies negative pressure in the oral cavity. This action moves the soft palate and tongue forward, increasing the upper airway’s size and decreasing the likelihood of collapse. In contrast to CPAP, iNAP eliminates the need for a mask over the nose or mouth, potentially enhancing comfort and adherence. Clinical studies demonstrate that iNAP significantly decreases apnoea events and enhances sleep quality in patients who cannot tolerate CPAP. The user-friendly design positions it as a promising choice, particularly for individuals looking for a less obtrusive treatment8.
3)Mandibular Advancement Devices (MAD)
For individuals who find CPAP intolerable, MADs offer a viable alternative. Oral appliances adjust the lower jaw forward while sleeping, enlarging the airway and minimizing obstruction by shifting the tongue base away from the throat wall. MADs are particularly beneficial for individuals with mild to moderate OSA and are recommended when CPAP is not well tolerated. Side effects may involve jaw discomfort or alterations in bite, yet in general, MADs provide a comfortable solution for many individuals9.
Upper Airway Surgery
Surgical interventions address the anatomical factors contributing to airway collapse. Procedures differ significantly, ranging from the removal of excess tissue to the repositioning of structures or the implantation of devices that stimulate airway muscles. A promising method is hypoglossal nerve stimulation, which uses an implant to intermittently activate the nerve that controls the genioglossus muscle, a pharyngeal dilator, enhancing airway patency during sleep. This approach addresses dysfunction in the pharyngeal dilator muscles and has demonstrated notable reductions in apnoea severity among specific patients. Surgery involves risks and varying success rates, typically considered only after non-invasive therapies have not succeeded10.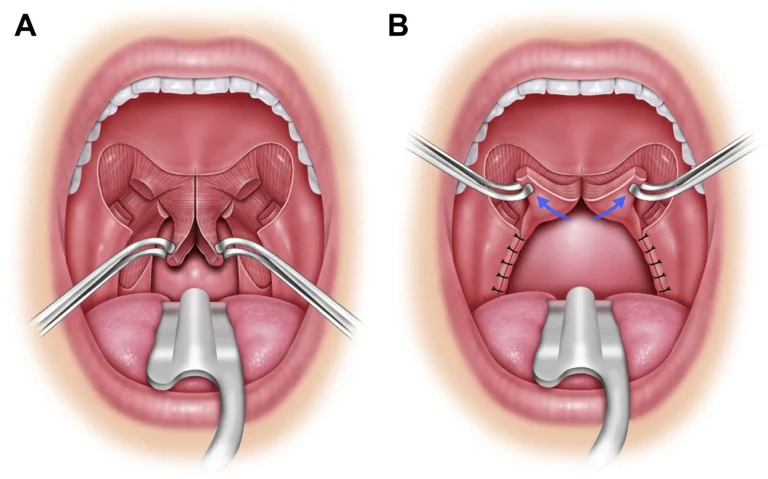
5)Nasal Expiratory Positive Airway Pressure Devices
These compact, adhesive devices generate positive pressure during exhalation, aiding in maintaining airway patency without the size of CPAP machines. They provide a convenient, portable option but are typically less effective than CPAP11.
7)Oral Pressure Therapy
This innovative treatment employs a vacuum system within the mouth to support the tongue and soft palate, effectively widening the airway. Initial research shows potential decreases in apnoea events, but further studies are necessary to validate long-term advantages12.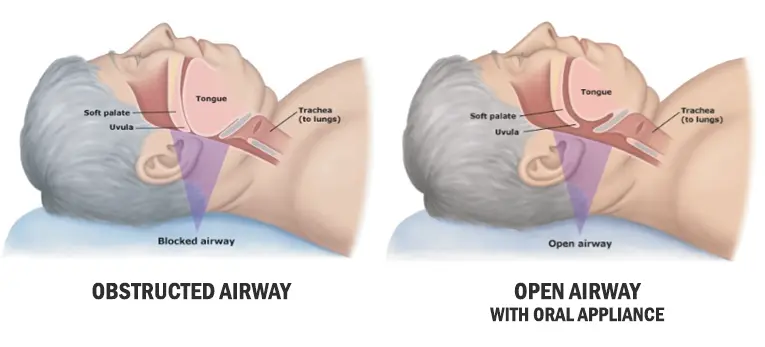
Why Awareness and Education Matter
Numerous individuals with sleep apnea go undiagnosed, as symptoms such as snoring and daytime sleepiness are frequently overlooked. Additionally, patients might be unaware of treatment options or may not fully appreciate the associated risks. It is essential to focus educational initiatives on both patients and healthcare providers. Enhancing knowledge of upper airway collapsibility, pharyngeal dilator muscle dysfunction, and other physiological factors can encourage individuals to pursue prompt diagnosis and treatment. Healthcare professionals, particularly ENT specialists, dentists, and sleep medicine experts, are crucial in increasing awareness, diagnosing, and effectively managing sleep apnea.
Conclusion
Sleep apnea is a common yet manageable condition that can lead to serious health issues if left untreated. Recent advancements in pathophysiology, including arousal threshold and ventilatory control mechanisms, have led to various treatment options beyond CPAP, such as upper airway surgery and innovative therapies. Consult a healthcare professional if you experience symptoms such as loud snoring, choking during sleep, or excessive daytime fatigue. Timely diagnosis and tailored treatment can significantly enhance sleep quality and overall health.
REFERENCES
- Benjafield AV, Ayas NT, Eastwood PR, et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: a literature-based analysis. Lancet Respir Med. 2019;7(8):687-698.
- Younes M. Role of respiratory control mechanisms in the pathogenesis of obstructive sleep disorders. J Appl Physiol (1985). 2008;105(5):1389-1405.
- Eckert DJ, Malhotra A. Pathophysiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):144-153.
- Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: an American Heart Association/American College of Cardiology Foundation Scientific Statement from the American Heart Association Council for High Blood Pressure Research Professional Education Committee, Council on Clinical Cardiology, Stroke Council, and Council on Cardiovascular Nursing. J Am Coll Cardiol. 2008;52(8):686-717.
- Punjabi NM. The epidemiology of adult obstructive sleep apnea. Proc Am Thorac Soc. 2008;5(2):136-143.
- Medical Advisory Secretariat. Polysomnography in patients with obstructive sleep apnea: an evidence-based analysis. Ont Health Technol Assess Ser. 2006;6(13):1-38.
- Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve. J Otolaryngol Head Neck Surg. 2016;45(1):43.
- Kuo YH, Liu TJ, Chiu FH, et al. Novel Intraoral Negative Airway Pressure in Drug-Induced Sleep Endoscopy with Target-Controlled Infusion. Nat Sci Sleep. 2021;13:2087-2099.
- Vecchierini MF, Attali V, Collet JM, et al. Mandibular advancement device use in obstructive sleep apnea: ORCADES study 5-year follow-up data. J Clin Sleep Med. 2021;17(8):1695-1705.
- Strollo PJ Jr, Soose RJ, Maurer JT, et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 2014;370(2):139-149.
- Berry RB, Kryger MH, Massie CA. A novel nasal expiratory positive airway pressure (EPAP) device for the treatment of obstructive sleep apnea: a randomized controlled trial. Sleep. 2011;34(4):479-485.
- Farid-Moayer M, Siegel LC, Black J. Oral pressure therapy for treatment of obstructive sleep apnea: clinical feasibility. Nat Sci Sleep. 2013;5:53-59.
