In busy Indian OPDs, many patients describe “giddiness” that looks similar at first glance, yet a swift distinction between vestibular neuritis and stroke can be lifesaving.
“An objective head impulse test methods make the decision clearer.”

Introduction
Across India, vestibular (inner-ear) problems are a leading cause of new-onset vertigo in clinics, with benign disorders like BPPV common. However, a meaningful proportion of patients also present with vestibular neuritis, demanding fast, reliable vertigo testing in primary and ENT settings. In one Indian multicentre registry, vestibular causes dominated new vertigo cases, while another Indian study reported vestibular neuritis in about 17% of vertigo patients seen in practice.1,2
Why this matters: confusing VOR dysfunction from a peripheral cause (e.g., vestibular neuritis) with a central cause (e.g., stroke) risks harm and delays care. Modern bedside and device-based tests, especially the head impulse test (HIT) and video HIT (vHIT) are central to getting the first decision right.3
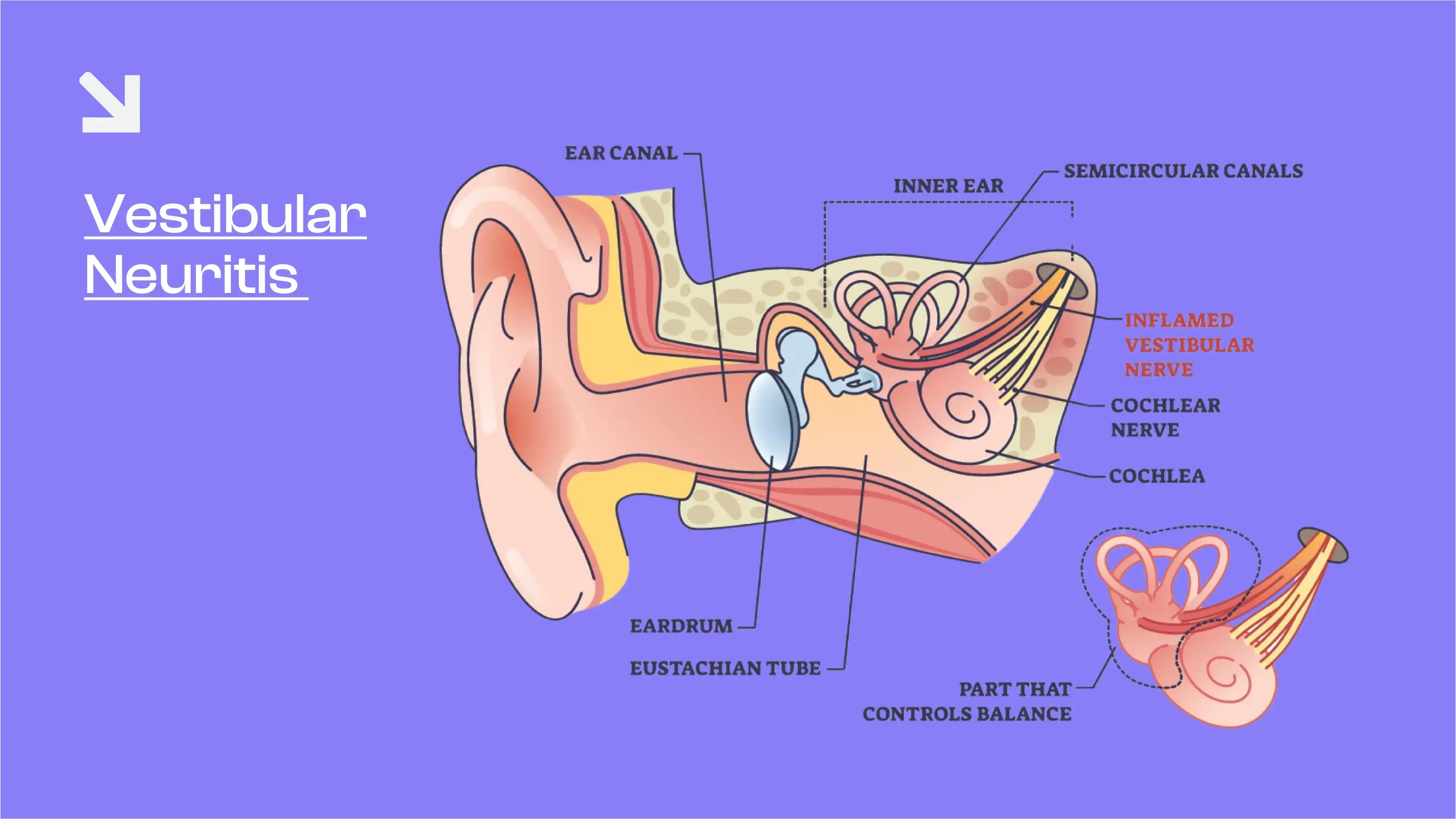
What is vestibular neuritis
Vestibular neuritis, also called acute unilateral vestibulopathy (AUVP), is a sudden loss of balance function on one side of the inner ear or its nerve, typically without new hearing loss. Patients feel continuous vertigo, nausea/vomiting, and imbalance, often with spontaneous eye movements (nystagmus). It is a peripheral disorder and part of the “acute vestibular syndrome.”4
In simple terms, your inner-ear sensors detect head motion and drive the vestibulo-ocular reflex (VOR) to keep vision clear when the head moves. If one side suddenly underperforms, the eyes cannot compensate properly, and because of VOR dysfunction, the world seems to spin.
Signs and symptoms to watch for
- Sudden, constant spinning or “giddiness” lasting hours to days
- Nausea, vomiting, and severe imbalance that worsens with head turns
- Blurred vision during head movement
- Red flags suggesting central causes (e.g., stroke): new double vision, weakness, severe headache, trouble speaking, requires immediate attention and emergency care.4
Risks of not detecting and treating
Missing a central cause (posterior-circulation stroke) can be dangerous. At the bedside, the HINTS battery and head impulse test improve early separation of peripheral versus central vertigo; device-based vHIT adds objective evidence of unilateral VOR loss typical of vestibular neuritis. Together, these reduce avoidable CT/MRI in low-risk patients while expediting imaging for those with stroke features.5
Current Diagnostic Landscape
- Head impulse test (HIT/vHIT): Measures the eye response to brief, unpredictable head turns in the plane of each semicircular canal. Reduced VOR “gain” and corrective saccades on the affected side point to VOR dysfunction from a peripheral lesion (e.g., vestibular neuritis). vHIT has been validated against search-coil gold standards and is widely used in clinics.6
- Limits to know: Early after symptom onset, some patients can show false-negative vHIT. Interpretation by trained clinicians is important and should be integrated with clinical signs.
- Other tests: Calorics, Vestibular Evoked Myogenic Potential (VEMP), audiometry, and targeted imaging support the overall picture when needed, but rapid, canal-specific testing at the point of care is increasingly preferred to triage effectively.
Innovation angle - Where EquiFHIT fits
EquifHIT (Functional Head Impulse Test) is a vestibulo-ocular reflex testing device that augments conventional vertigo testing by linking physiology to function. Instead of only tracking eye movements, EquiFHIT asks a simple, patient-relevant question at the exact peak of head velocity: can the patient recognize a briefly shown optotype (letter/symbol) while the head is turning fast? This demand stresses the VOR precisely when it must perform.

Key capabilities from the source:
- Head-mounted high-precision sensors measure angular velocity in three planes -horizontal, LARP, and RALP, for canal-aligned testing.
- Peak-velocity timing: The optotype appears only at peak head speed and disappears as velocity drops, ensuring results truly reflect real-world VOR demands.
- Smart rejection: Suboptimal presentations are automatically discarded for clean data.
- Inclusive optotypes: Standard Snellen letters and Landolt C symbols help test both literate and non-literate patients, useful in Indian practice.
- Per-canal scoring & color coding: Results show the number correct out of 10, with green/yellow/red indicators and auto-generated, canal-wise reports that clinicians can read at a glance.
Why does this help in vestibular neuritis
- Unilateral mapping: Because vestibular neuritis usually affects one side, EquiFHIT’s canal-specific approach can reveal lower functional performance in horizontal-canal trials on the affected side, mirroring the unilateral VOR dysfunction that vHIT quantifies.
- Function + physiology: Patients don’t just produce traces; they either identify the optotype or not at peak velocity. This makes the result easy to explain to families and actionable for therapy planning.
- Workflow ready: Setup, trial quality control, and automatic reports are designed for busy OPDs.
How EquifHIT complements today’s head impulse test
Consider a patient with acute continuous vertigo, no hearing symptoms, and abnormal bedside HIT to the right.
- vHIT may show reduced horizontal-canal gain and corrective saccades on the right, typical for vestibular neuritis.7
- EquiFHIT tests the same canal planes but asks for optotype recognition at peak head velocity; poorer scores on rightward impulses provide a functional correlate of VOR dysfunction that’s easy for non-specialists to understand, strengthening the case for a peripheral diagnosis when integrated with exam findings.
Practical Notes for India
- Burden & patterns: Indian clinic data consistently show vestibular disorders as a major share of new vertigo; vestibular neuritis represents a meaningful subset in real-world practice.1
- Access & literacy: EquiFHIT’s use of Landolt C makes vertigo testing practical when English literacy is limited, improving inclusivity in diverse communities.
Call to Action
Patients & caregivers: If continuous spinning, severe imbalance, or blurred vision with head turns begin suddenly and there is no new hearing loss, seek prompt evaluation. Early head impulse test and vertigo testing help separate vestibular neuritis from stroke.3,4
General practitioners & referring physicians: For acute vestibular presentations without red flags, consider early HIT/vHIT and ENT referral. Adding functional tools like EquiFHIT can clearly document unilateral VOR dysfunction, support the diagnosis, and guide vestibular rehabilitation.5
Clinics & hospitals: Integrate EquiFHIT alongside your vHIT to obtain both quantitative gain and function-linked scores, with per-canal automated reports for longitudinal tracking.
For complete information and to request a demo of EquiFHIT, navigate through EquiFHIT. To contact Taevas Global and for a quick support, dial +91 87654 22222
References
- Kameswaran, M., Pujari, S., Singh, J., Basumatary, L. J., Sarda, K., & Pore, R. (2017). Clinicoetiological pattern and pharmacotherapy practices in patients with new onset vertigo: Findings from a prospective multicenter registry in India. International Journal of Otorhinolaryngology and Head and Neck Surgery, 3(2), 404–413. https://doi.org/10.18203/issn.2454-5929.ijohns20171202
- Kameswaran, M., Bharathi, M. B., Periera, C., Chandra, S., Reddy, H. K., Gupta, M., Sholapuri, D., & Peethamabaran, K. (2023). Effectiveness and Safety of Prochlorperazine in Indian Patients with Acute Vertigo: Results from a Large, Prospective, Post-marketing Observational Study. Indian journal of otolaryngology and head and neck surgery : official publication of the Association of Otolaryngologists of India, 75(4), 3152–3160. https://doi.org/10.1007/s12070-023-03831-0
- Jaganathan, N., Mohamed, M. H., Md Pauzi, A. L., Mahayidin, H., Hanapai, A. F., Wan Sulaiman, W. A., Basri, H., & Inche Mat, L. (2024). Video head impulse test in stroke: a review of published studies. Frontiers in neurology, 15, 1339039. https://doi.org/10.3389/fneur.2024.1339039
- Strupp, M., Bisdorff, A., Furman, J., Hornibrook, J., Jahn, K., Maire, R., Newman-Toker, D., & Magnusson, M. (2022). Acute unilateral vestibulopathy/vestibular neuritis: Diagnostic criteria. Journal of vestibular research : equilibrium & orientation, 32(5), 389–406. https://doi.org/10.3233/VES-220201
- Wang, C., Sreerama, J., Nham, B., Reid, N., Ozalp, N., Thomas, J. O., Cappelen-Smith, C., Calic, Z., Bradshaw, A. P., Rosengren, S. M., Akdal, G., Halmagyi, G. M., Black, D. A., Burke, D., Prasad, M., Bharathy, G. K., & Welgampola, M. S. (2025). Separation of stroke from vestibular neuritis using the video head impulse test: machine learning models versus expert clinicians. Journal of neurology, 272(3), 248. https://doi.org/10.1007/s00415-025-12918-3
- Welgampola, M. S., Halmagyi, G. M., Snapp, H. A., Schubert, M. C., Crowson, M. G., & Straumann, D. (n.d.). *Head impulse test*. ScienceDirect. https://www.sciencedirect.com/topics/medicine-and-dentistry/head-impulse-test
- Jasinska-Nowacka, A., & Niemczyk, K. (2024). Application of a Video Head Impulse Test in the Diagnosis of Vestibular Neuritis. Life (Basel, Switzerland), 14(6), 757. https://doi.org/10.3390/life14060757