Why Vestibular Rehabilitation Is Crucial After Inner Ear Damage
Studies suggest that dizziness and balance disorders affect about 15-20% of adults at some point, with higher prevalence in people over the age 40.1 In India, conditions like labyrinthitis (inner ear infection), vestibular neuritis, and head injuries are leading causes of chronic dizziness and unsteadiness.
What is vestibular rehabilitation?
The vestibular system, located deep within the inner ear, acts like a gyroscope of our body. It helps detect movement and head position. When it is damaged, it is like a ship losing its compass and moving without a clear sense of where we are headed. Every decision feels uncertain, and even progress can feel aimless.
Vestibular rehabilitation therapy (VRT) is a specialized, exercise-based program that retrains the brain to compensate for inner ear damage.2 It involves targeted head, eye, and body movements to:
- Reduce dizziness
- Improve balance
- Restore confidence in movement

Common symptoms after inner ear damage
- Persistent dizziness or vertigo
- Unsteady walking, especially in the dark
- Feeling “pulled” to one side when standing or walking
- Difficulty focusing eyes when moving the head (blurred or jumping vision)
- Nausea or motion sickness
- Anxiety about falling
Risks of not detecting and treating
Without timely vestibular rehabilitation:
- Chronic imbalance – leading to dependence on walking aids
- Increased fall risk – especially in older adults, causing fractures or head injuries
- Reduced independence – avoiding crowded places, travel, or stairs
- Depression and social withdrawal – due to persistent dizziness
- Delayed recovery – as the brain fails to adapt naturally
In older adults, untreated vestibular dysfunction can double the risk of falls, a leading cause of disability in India.

Current diagnostic landscape
In many clinics, dizziness is assessed using:
- Patient history and symptom description
- Bedside balance tests (Romberg, Dix-Hallpike)
- Hearing and inner ear function tests
- Imaging (MRI/CT) to rule out brain lesions
While this helps identify causes, treatment is often limited to medications like anti-vertigo drugs, which may relieve symptoms but do not restore long-term balance control.
What’s changing - The innovation angle
Modern vestibular rehabilitation goes beyond generic balance exercises. Programs are now individualized based on the patient’s deficits.
Key advances:
- Computerized posturography – Platforms like EQUIPOISE measure body sway in real time, identifying subtle balance deficits for targeted therapy.
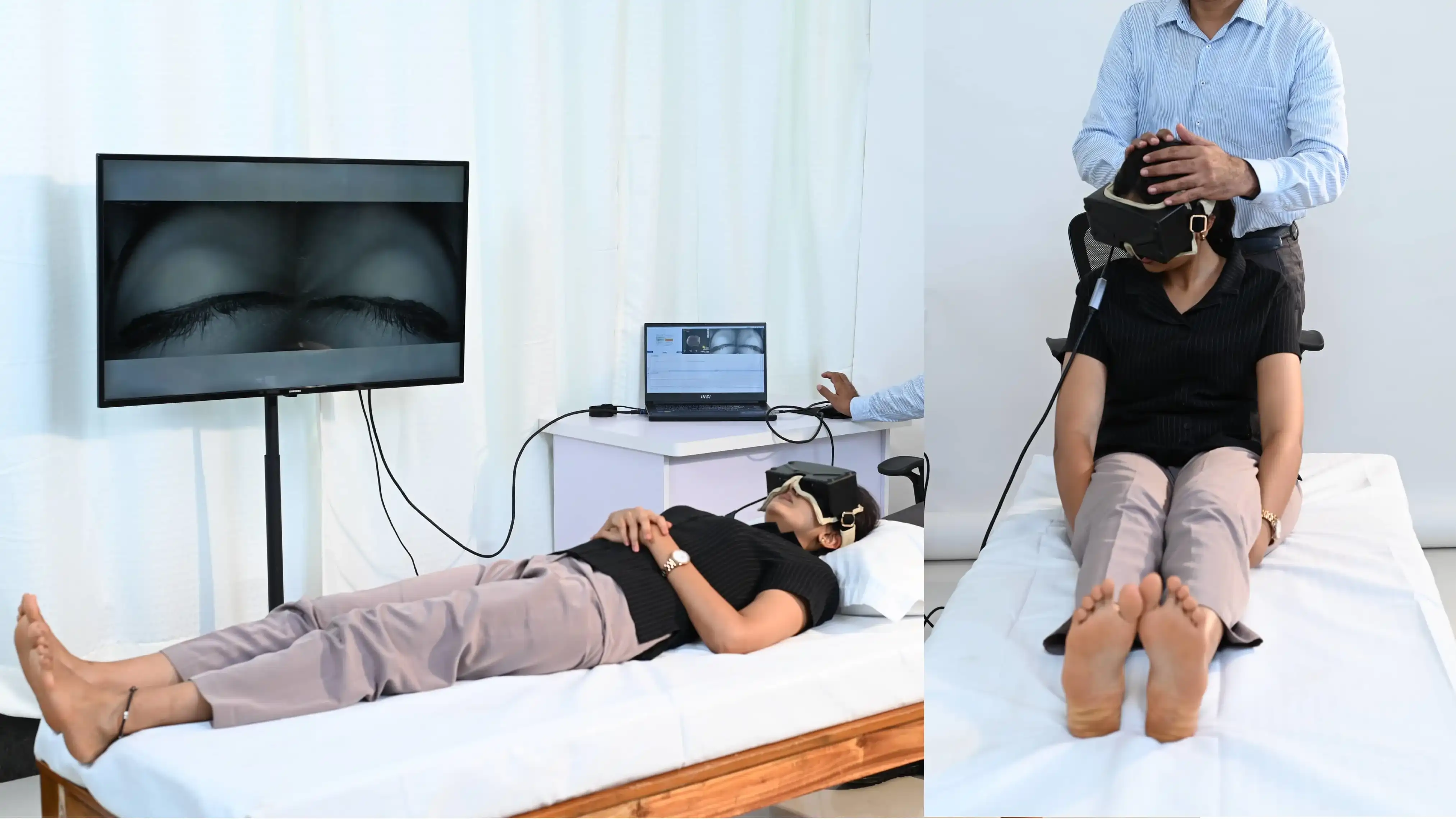
- Computer vision systems (e.g., EquiCCG) – Use high-resolution cameras to assess nystagmus, gait and postural control.
- Virtual Reality (VR) therapy – Simulates motion-rich environments to help the brain adapt safely.
- Tele-rehabilitation – Remote sessions for patients in rural areas, guided via video and wearable sensors.
A recent study by Joshua et al. 2022 found that vestibular rehabilitation significantly improves balance scores within 6 - 8 weeks of consistent therapy, even in chronic cases.4
Vestibular rehabilitation exercises – what they involve
A trained vestibular physiotherapist will design a program that may include:
- Gaze stabilization: Moving the head while keeping eyes fixed on a target.
- Habituation exercises: Gradually exposing the patient to movements that trigger symptoms.
- Balance retraining: Standing and walking tasks on varied surfaces.
- Functional activities: Simulating daily tasks like turning quickly or bending.
Progress is monitored, and exercises are adjusted as the brain adapts.

Call to Action
If you or your loved one:
- Have had recent inner ear infections or head trauma,
- Feel persistent dizziness or imbalance,
- Avoid activities for fear of falling,
It’s time to talk to your doctor about vestibular rehabilitation.
With EquiPoise, EquiCOG, EquiCCG, and EquifHIT, your clinician gains the rapid, objective data needed to tailor treatment and guide you back to stable balance.
Take control of your balance today: visit Taevas Life Sciences to download our brochure or call +91 87654 22222 to schedule a hands-on demonstration.
Early therapy can mean the difference between living cautiously and moving confidently.
References
- Neuhauser HK. The epidemiology of dizziness and vertigo. Handb Clin Neurol. 2016;137:67-82. doi: 10.1016/B978-0-444-63437-5.00005-4. PMID: 27638063.
- Tsukamoto, H. F., Costa, V.deS., Silva, R. A., Junior, Pelosi, G. G., Marchiori, L. L., Vaz, C. R., & Fernandes, K. B. (2015). Effectiveness of a Vestibular Rehabilitation Protocol to Improve the Health-Related Quality of Life and Postural Balance in Patients with Vertigo. International archives of otorhinolaryngology, 19(3), 238–247. https://doi.org/10.1055/s-0035-1547523
- World Health Organization. “Falls.” WHO Fact Sheet, 2021.
- Joshua, A. M., & Pai, S. (2022). Vestibular rehabilitation. In A. M. Joshua (Ed.), Physiotherapy for adult neurological conditions (pp. 495–538). Springer. https://doi.org/10.1007/978-981-19-0209-3_7